Following a one week trip home to California, I returned to Houston on January 22nd to prepare for my mastectomy on January 24th. However, at my pre-op appointment on the 23rd, I learned that my blood work had produced an obstacle to preceding. Stable throughout chemotherapy, my platelets had taken a big drop. Other important factors for healing were not within safe range, either, so surgery was postponed until 1/29th. But, once again when my pre-op blood work indicated surgery would not be prudent on the 29th due to low platelets and low white blood counts, I was rescheduled for February 5th.
These two delays due to Thrombocytopenia, “an abnormally low amount of platelets…[the blood cells] that help wounds heal and prevent bleeding by forming blood clots,” as well as low white blood counts important for healing, found me walking that thin line between disappointment for the deferral, and relief for such a thorough, conscientious and caring surgeon. While both delays were initially disappointing, I quickly came to accept and appreciate why they were necessary, and to comprehend how critically important trust and confidence in ones medical team is to mitigating the prevalent apprehension and concerns connected to a cancer diagnosis and treatment. When delays induced in me a dread that the cancer could possibly gain a new foothold or metastasize while we waited for my platelets and Absolute Neutrophil Count (ANC) to rise, or that I could suffer serious, or even fatal complications if my body weren’t strong enough for surgery, I composed and calmed myself with deep breathing, meditation, and prayers of gratitude for my many personal blessings; I am being treated at MD Anderson, the preeminent cancer center in the nation, by leading medical experts in their respective fields, and could not be in better hands.
Throughout much of my chemotherapy treatment I had suffered from anemia and neutropenia, or too few absolute neutrophil (ANC) cells. “These cells are made in the bone marrow and travel in the blood throughout the body. They sense infections, gather at sites of infection, and destroy the pathogens.” Conversely, my platelets had remained in the normal range throughout treatment…at least until they took a dive following my final AC infusion. Some 4-5 weeks following my last chemotherapy treatment, I just wasn’t rebounding. This unexpected circumstance took my care team and me by surprise, to say the least. Were my platelets plummeting due to some as yet undiscovered, or newly manifested malignancy? Under my surgeon’s, Dr. Mediget Teshome, conscientious and comprehensive care, I was referred to Dr. Thein Oo, an MD Anderson hematologist, to rule out any serious underlying conditions. Dr. Oo discerned from additional blood tests that while low, my platelets were stable enough for surgery. But, he was concerned about my low ANC. After consulting with Dr. Teshome, it was decided I would receive two Neupogen shots over the weekend to boost my white blood count, and undergo a platelet transfusion at the time of surgery. I finally underwent a modified radical mastectomy on February 5th.
The surgery lasted some 4+ hours, as my surgeon meticulously ensured the integrity of the sites against internal bleeding, particularly where copious tiny blood vessels connected the 22 removed lymph nodes. Sister, Sally Jo, acted as my overnight hospital advocate; she was a force to be reckoned with when it came to my pain management, waking all night to hydrate and comfort me.
*WARNING* the next 2 pictures are graphic and VERY early in the healing process, so if you’re uncomfortable seeing the consequences of a modified radical mastectomy, scroll quickly down to the “GO” sign. Keep in mind the scar will change color and flatten as it heals. The tubes emerging from my side drain fluids into small bulbs, which are measured and emptied twice per day.

I remained in the hospital a couple of nights for observation, then sent home to heal up and prepare for radiation.
Nephew and niece, Eric and Natalie, insisted I stay at their home, where I could be monitored and assisted by Natalie, a Nurse Practitioner. Neal was headed home to California on Saturday, 2/10, and like me, very grateful for their invitation. What could be better than the adorable entertainment at the “von Wenckstern Recovery Center”? It would turn out to be a fortuitous choice.
On 2/13, I learned my pathology report results. Chemotherapy had been only somewhat effective at evicting this uninvited interloper, leaving behind “invasive tumor cellularity averaged to approximately 40%, and “metastatic carcinoma present” in 5 of the 22 total lymph nodes removed. Not the outcome anyone was hoping for, of course…I was devastated.
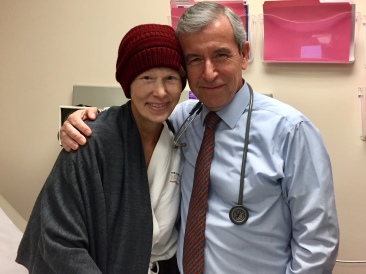
But, as my oncologist, Dr. Vicente Valero, finished delivering the news and I began to cry, he held my hands and cautioned me not to “focus for too long on these numbers, or what we haven’t yet achieved.” He assured me and my family that he and his team are already working on what intervention(s), in addition to radiation, may be available to me. While acknowledging my right to feel disappointed and upset about the pathology report, he also encouraged me to maintain a more future-oriented outlook. “You still have options,” he explained.
Loved ones, medical care providers, and even strangers encourage me to maintain a positive attitude…a state of mind I believe I’ve always possessed; an inherent temperament my mother contended was evident at birth, when laid upon her breast I, “looked up and smiled” at her. It is this optimistic, cheerful attitude, I assume, that was responsible for the childhood nickname, “Jolly,” bestowed upon me by my “best, good friend” Lisa (Horn) McQuordale’s step-father, Rudy.
As I crumbled, I would have loved to pull out my “positive attitude” cape and transform into “Jolly.” Instead, I was overcome by deep despair. Fortunately, I had some of my awesome cancer support crew there to comfort and console me.
And, there was one bright spot: my estrogen receptor status changed from negative to 20% positive, allowing use of hormone therapy “to stop estrogen from attaching to the receptor cell.”
At that point, I was still weak, fatigued, in pain, and needed to heal from a 4+ hour surgery just 8 days prior, which would soon prove problematic, and require yet another hospital stay for a post-surgical infection.
On Wednesday evening, 2/14, As Natalie helped me strip the tubes and measure drain output the pain suddenly spiked along my incision sites. I became very dizzy and suddenly threw up in the sink. It was a bizarre and never-before-experienced effect. I had just seen my doctors the prior day. I had been closely examined and showed no signs of infection. I was scheduled to have one of my drains removed the following morning, 2/15.
Once past the episode, Natalie checked my temperature, which was normal. I took my evening meds, went to bed, but tossed and turned all night. I arose around 6:15 am on February 15th, to prepare for my appointments at MDACC. I felt horrible. Natalie checked in on me before departing for work, and as she hugged me goodbye, she said, “Aunt Jill, you’re very warm. We need to check your temperature.” It was 101.8. Natalie said, “You’re most likely going to the emergency room, so just be prepared.” She helped me pack my bag, and sent me off with Eric. On the way to the hospital, I texted my surgeon to inform her of my temperature and to inquire whether I should keep our 8:00 am appointment, or go to the emergency room. She texted back that she wanted me to come see her first. When we arrived at the Mays Clinic, Eric dropped me at patient drop-off and went to park. As I shuffled slowly to the elevator, feeling 100 years old, a woman’s voice called to me, “Are you tired, ma’am, or weak?” I turned around to answer the woman, a nurse, who sat me in a chair and told me to wait while she retrieved a wheelchair. She delivered me to the Breast Clinic on the 5th floor, where I had the wherewithal to ask her to take a picture with me…evidence that there are always angels in our midst…

When I was called back for vitals, the nurse first measured my blood pressure in the 60’s. She rechecked it to be certain, recording: 78/51…a new low for me. My temperature was normal, as I had taken 2 extra strength Tylenol prior to leaving. I was dizzy and short of breath. Upon examination by my surgeon, I was referred to the emergency room. Eric wheeled me over to MDACC’s main building in a wheelchair. I refused to be transported in an ambulance. After being tested and treated in the emergency room for hours, I was admitted to the ICU. Eric never left my side, keeping family informed, and strongly advocating for me amongst all the chaos. He slept by my side that first evening in one of those oh-so-comfortable hospital chairs. And, I have no evidence, but Dr. Teshome may have temporarily moved into a room at MDACC for the next several days. Eric asked me at one point, “Has Dr. Teshome even gone home at all?” I had to wonder, as she was at my bedside so often informing me about my most current status, her concerns, plan of action, and to expect visits from the additional specialists with which she was conferring.

I was diagnosed with Post Mastectomy Lymphedema Syndrome, Cellulitis and Sepsis. “Cellulitis is an infection of the skin and deep underlying tissues. Group A strep (streptococcal) bacteria are the most common cause. The bacteria enter your body when you get an injury such as a bruise, burn, surgical cut, or wound.” My white blood count, notoriously low, had shot up. On the one hand, it was a positive indicator that my body was attempting to mount a defense. But, it was also a symptom of Sepsis, “…a serious illness [that] happens when your body has an overwhelming immune response to a bacterial infection…Anyone can get Sepsis, but the risk is higher in people with weakened immune systems.” It was frightening, and frankly stunning how quickly the infection developed and sickened me. Thank G-d for my smart, observant niece, “big guns” antibiotics, and the comprehensive medical care I am blessed to access.

I remained in the ICU for a couple of nights of stabilization, more tests, fluids, and another blood transfusion before being moved back to the post-surgical floor where, with the help of my awesome nurses, and family, of course, I continued to recover.
I was released from the hospital on 2/22, with a portable antibiotic machine that I will wear for 7 days, scar tissue stretching exercises and a massive sigh of relief. Neal assists me with all my tubes and antibiotic machine, takes me for walks through the neighborhood, shops and cooks for me, provides medication throughout the night, and generally keeps me amused with his musical choices. After I complained about mobility, balance issues, and trying to squeeze into compression socks due to swollen legs, ankles and feet, Neal played the song, “Funky Cold Medina, on the JBL speaker, singing the refrain, of course, as “Funky Cold Edema.” Laughter truly is healing…the swelling is receding.
I was asked during my MD Anderson physical therapy assessment how I would rate my quality of life. I said, “Well, today (the day of my pathology report results), I received some pretty disappointing news I haven’t fully processed. But, even with that report in mind, and despite the fact I have cancer, I’d have to rate my quality of life as excellent.”
Considering my blessings: a wonderful husband whom I love and adore, and who has taught me about trust, contentment, forgiveness, and the profound bond possible between two people; two sons who are the absolute light of my life, and the best thing I’ve ever done – aside from marrying their father; (too many) pets that provide great joy, amusement and the kind of “unconditional love” we humans can only strive to emulate; a large, loving family and kind, thoughtful friends whose generosity, help and unwavering support nourish my soul; and premier medical care at the leading cancer facility in the nation…Yeah, I’d have to say my quality of life unquestionably rates in the excellent range.

I’m just terribly homesick…and, frightened about the future…How much future there is for me…what it will look like…how my family will continue to be affected by my disease…and, by my absence.
The chaplain who visited me in the hospital as I recovered from the post-surgical infection asked, “If G-d were here in this room with you now, what would you ask Him for?” I began to sob, reverting to a small child whose innermost, fondest, but long-stifled wish was finally being heard by someone who would not feel overwhelmed by, or the need to interrupt or regulate my emotional exposure and vulnerability. “Time,” I whispered, faintly. “I just want more time. I’m not ready to go. I don’t want to leave my family.”
Fighting Inflammatory Breast Cancer these past 8 months has made it challenging, to say the least, to sustain my normal level of positivity each and every day, or even for an entire day. In the often long and arduous campaign to kill a cancer, a predominantly positive attitude may find more footing in a less taxing treatment regimen, or against a less aggressive opponent…It may be manageable to feel consistently hopeful and optimistic, I imagine, when ones cancer has a high survival rate, has more treatment options, or when therapy proceeds without unremitting, debilitating side-effects, infections, or setbacks. It’s a whole ‘nother story when you frequently feel so sick and fatigued that sedentariness, the antithetical disposition of your former self, becomes your new normal. Or, when your side-effects create so many setbacks your treatment is frequently delayed. Or, when there are less treatment options available. Or, when your cancer type is more associated with death than survival. Or, when your best chance for at least 2-10 more years requires moving to another city…without your spouse or sons. I am as positive as I possibly can be under my current circumstances.
I still believe I have more years ahead of me. It’s the not-knowing how many that keeps me awake at night, and exposes my abject terror. Some people respond to my stated fears with, “Well, none of us know how much time we have left.” While I realize that’s true, conjecture about life expectancy in a broad or general sense is far from comforting to someone facing a deadly disease that won’t surrender despite an often grueling chemical assault that included four potent, powerful chemotherapy agents and one of the promising monoclonal antibodies, a relatively new type of “targeted” cancer therapies.
My team has informed me of another trial study, located exclusively at MD Anderson, for which I may be eligible. “The goal of this clinical research study is to learn if Pembrolizumab (Keytruda) in combination with standard hormone therapy can help to control and prevent IBC. The safety of this drug combination will also be studied. Pembrolizumab is FDA approved and commercially available for the treatment of metastatic melanoma. Its use in patients with IBC in combination with standard hormonal therapy is considered investigational.” If I qualify, my family and I will be faced with new, additional and immensely difficult decisions.
When people tell me I’m “strong” to seek treatment so far away from home, I think, “Not really. You have no idea how often I feel frightened, distraught, vulnerable and weak.” I live with an interminable internal conflict over whether this time away from my husband and sons will have been worth it. Perhaps the strength people refer to is the fact that I just buck up and do it, because I want to live. In that case, I guess none of us really know how “strong” we can be until we have no choice.
I made a conscious, aware and informed decision to trade a year of displacement and separation from my husband and sons for the opportunity to marvel a while longer over the vast magnitude of all G-d’s creation, to prolong the life-affirming feelings of love and devotion I’ve been blessed to share with my family, to dance at my sons’ weddings, and to slowly inhale the sweet, sweet scent of my future grandchildrens’ brand new, tiny heads and soft, velvety skin.
Qualifying for the trial at MDACC means trading even more time away from my home versus a possible chance at extended longevity; more investigational therapy that will, no doubt, sicken me… and may or may not prove effective. But, before I decide, I must first get through radiation…
Then, somewhere in peaceful, quiet repose, I trust the answer will come to me.

























Praying for you, sweet lady!
It is perfectly normal to feel abject terror at a time like this – you’re facing some really scary stuff. Please know that people are here to bolster you and to hold you safe those times when you just can’t deal with it anymore.
People who have never been there don’t understand that in these situations, a person is “strong” because they don’t have any choice but to confront things head-on. It’s not because that is what they WANT to be, it just is what it is.k
Great big hugs to you, dear one.
LikeLiked by 1 person
Thank you, Teresa. Wise words from someone who understands the “strength” it requires to face an incomprehensible challenge for which we have no training, no experience, and no other choice but to confront if we are not ready to surrender. It is the love and support of family and friends that carries me through. Much love to you and your family. ❤️
LikeLike
Jill,
Your words are powerful and the specific details add deeply to our understanding of your unique suffering. Even as a physician of 33 years in primary care, I find your story intensely moving and humbling; although I can’t imagine even a seasoned cancer doctor habituated to the practice of peddling various chemo poisons wouldn’t feel the same. It certainly puts into perspective the small and obviously trivial frustrations that sometimes get us stuck. My heart goes out to you along with my hopes that one of these investigational bullets will stop this dreaded disease.
Love always,
Brian
LikeLiked by 1 person
Thank you, Brian. Much has been put into perspective, that’s for certain! As always, I so appreciate your thoughtful words and wise counsel…especially as a physician in this case! Your love and support, not just for me, but for Neal has been a blessing. I can’t tell you how much it means to me to know Neal has you in his corner. Much love to you and the family. ❤️
LikeLike
Jill. Your words and story are so powerful. I have tears in my eyes. I admire your bravery and strength. I am so blessed to have met you and your husband. I’m praying for you and know you are a survivor. 🤗🤗💕💕🙏🙏🌺🌺. Sending you a big hug and love Jill
LikeLike
You’ll always have that cheery attitude. I can’t imagine you wouldn’t. I know you can beat this horrible disease. Not a question in my mind. My prayers for your speedy recovery are always put out in the universe. And when you’re recovered I’ll keep praying it stays that way. I really love you. You’re the nicest sweetest person I know. And yes I do mean that. I’ve known you from a distance for over 20 years. I’m just sorry I don’t go to CA that much. But, if I had you just might have just gotten sick of me lol. Keep up your positive attitude and zest for life.
And I love the fact you have a million pets lol. As do I lol. I love you Della. Oh, if you need anything I mean ANYTHING please let me know and I’ll have it to you right away.
LikeLiked by 1 person
Hey there you kind, intelligent, hard-working and beautiful inside and out woman! I’m getting such a kick out of the photos of your new puppy! LOVE that you have a houseful of dogs now…I’m hanging in there. Neal is here, so that helps. I would never get sick of you! lol…I love your words of support and prayers, my friend…Thank you! ❌⭕️ ❤️ 🙏🏻
LikeLike
And here I am in tears again……. Your words are so raw and provide such powerful lessons for those of us not physically fighting the battle you are engaged in right now. Sending love and strength your way as always. Can’t wait to see you again soon!! Love you, Julie
LikeLiked by 1 person
Hello sweet Jill!!
I love reading your posts while it breaks my heart, it gives me a few moments to stop everything and think only of you, your struggle and strength! I can hardly wait to see and hug you again while we celebrate the end of your journey. ….And then to look forward to the pictures of you dancing at your adorable son’s weddings!! Big hugs, lots of love!! Debbie
LikeLiked by 1 person
Hi Debbie! So good to hear from you! I hope this finds you and yours healthy, happy and enjoying sunny soCal! I know you’re probably as busy as ever, so thanks for taking the time to read my blog and to respond…I miss you and our Hot Yoga 1000 women’s locker room “post-class-survival” conversations! My love right back at you! ❤️
LikeLike
Jill, you are and forever will be the bravest and most wonderful person we have ever met. Since having you here for A. L. Chafin meet, you have never been very far from our hearts.
Now waiting for you and family to come back. Love and future, Jerrel and Joan
LikeLiked by 1 person
Dearest Joan and Jerrel, I was just speaking to Neal of you and my fond memories of our time together. From our wonderful conversations during our long drives, around the kitchen and dinner table, to your kind and generous hospitality, I felt an instant connection and love for your both…as if I’d known you all my life. I think of you often, and have a visit to you on my “to do” list when I recover. Miss you and love you much…❤️
LikeLike